After earning her Master of Science in Nursing at Vanderbilt University in 2016, Caitlyn White began her career as a nurse practitioner (NP) in Fort Worth, Texas. There, she worked with a group of nine pediatricians and neonatologists to oversee the care of newborns from their birth until their discharge home. While practicing in Texas, White was subject to some of the strictest scope of practice (SOP) laws in the country, which govern how physicians oversee midlevel providers.
For White, these laws meant that almost all of the medical charts and diagnoses she completed had to be reviewed by her supervising physician. She also legally could not practice unless her supervising physician was either on-site or less than 15 minutes away. In her view, these regulations were never beneficial. Rather, they were simply burdensome for both her and her supervising physician.
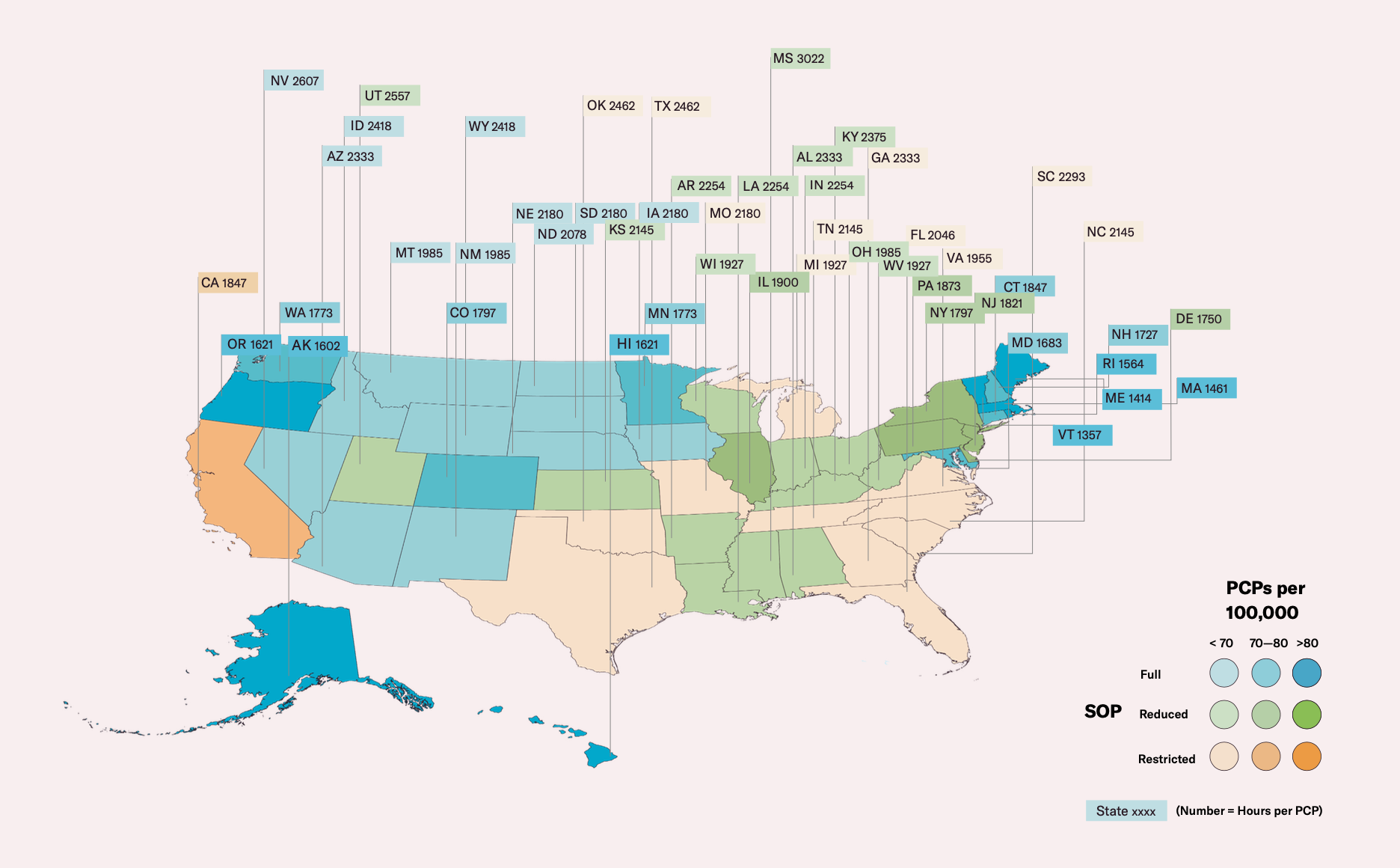
Now practicing in Massachusetts, where there are much less stringent SOP laws, White is often the only professional at her practice on weekends. Until recently, she needed to have an on-call physician available, but now even that is not required. In January of this year, the governor of Massachusetts issued an emergency executive order in response to Covid-19 to grant NPs Full Practice Authority (FPA), giving NPs the ability to operate with complete independence and care for their own patients. Massachusetts became only the 23rd state in the United States to grant FPA. The evidence suggests that if the United States is going to fix its primary care system, other states should follow suit.
White believes that trust is what has made her experience as a provider in Massachusetts different than in Texas. Operating with virtually no oversight, she no longer feels like a physician is always behind her and looking at what she is doing. According to White, “it’s like having two different careers.”
Given how much the designated responsibilities of a nurse practitioner can vary by state, it is worth noting what NPs are actually trained to do. NPs are advanced practice nurses that prescribe medications, examine patients, order tests, diagnose illnesses, and provide treatment. Before practicing, NPs must earn a Bachelor of Science in Nursing, become a certified registered nurse, complete a Master of Science in Nursing, pass a national exam, and gain state licensure. Together, this totals between six and eight years of education and training, in comparison to the 10 to 14 years needed for Doctors of Medicine (MDs).
This difference in training is a commonly cited reason in support of NP oversight by supervising physicians, though study after study shows that care provided by independent NPs is on par with care provided by MDs, especially in primary care settings. In a 2019 study on patient satisfaction, survey results from more than 50,000 patients showed that patient satisfaction may even be higher for patients who see NPs when compared to MDs in primary care provider (PCP) roles. Specifically, the communication skills of NPs were rated slightly higher than those of MDs, perhaps due to longer consultations or better listening.
The ability of NPs to take on the role of autonomous PCPs is highly relevant to the future of healthcare in the United States. Trained as generalists, PCPs are a patient’s first point of contact for any medical concern. They are the providers with whom patients generally have the strongest and longest relationships. It is no surprise that a higher ratio of PCPs to population size is significantly associated with lower mortality. Currently, there are only about 200,000 PCPs practicing in the United States, and the average wait time in large cities to see a PCP is already steep at 29.3 days. However, with an aging population and a PCP workforce that graduating MDs are failing to replenish, the United States will be short 50,000 PCPs in the next decade if nothing changes.
Despite this impending shortage of PCPs, the NP workforce in the United States is growing rapidly, having more than doubled since 2013. Contributing to this growth is the fact that the number of graduating NPs each year is now about equal to that of graduating MDs. While less than a third of physicians practice in primary care, 84 percent of NPs are trained in primary care and 78 percent of all NPs currently deliver primary care. Importantly, a far higher percentage of NPs also choose to practice in rural or underserved communities.
The growing NP workforce will be an important part of the solution. As NPs remain subject to physician oversight, the impact of their care is greatly restricted. Primary physicians have an extensive set of responsibilities: Not only do they spend 33 hours each week in direct contact with their patients, but they also must review all charts and diagnoses made by NPs, who usually see three or more patients per hour. As such, physicians are limited by these burdens and often must spend less time with patients in order to buy themselves time to review work done by NPs. This effort is largely duplicative and reduces access to care.
Required on-site supervision or set distance limits reduce organizational capacity, too. Evidence has shown that in states with the least restrictive SOP laws, patients are 2.5 times more likely to receive care from an NP than in states with the most restrictive SOP laws. With ample data demonstrating the quality of NP primary care, existing regulations are simply outdated.
Still, some physicians cling to SOP laws. As White notes, there are “a lot of fight[s] between NPs and MDs” over SOP laws, leading to large-scale lobbying in support of physician oversight from organizations such as the American Medical Association. NPs are a growing workforce and demand lower salaries. Physicians fear displacement and argue that NPs are not adequately trained to be fully independent decision makers, even though that is not necessarily the goal of deregulation. However, White insists that “you’d be hard-pressed to find a midlevel who doesn’t appreciate collaboration.” She also does not see NPs as attempting to isolate themselves from other providers, as this would not reflect the general trends in primary care. In fact, across the board, team-based care models are gaining popularity.
Since the start of the pandemic, governors from Wisconsin, Michigan, Tennessee, and Pennsylvania have all temporarily deregulated restrictive SOP laws to increase providers’ capacity to handle an influx of patients. However, access to healthcare in the United States is not just a problem because of Covid-19. Compared to other Organization for Economic Co-operation and Development countries, the United States spends the most on healthcare and has the highest rate of avoidable deaths. Nearly two-thirds of bankruptcies in the country are due to medical expenses; meanwhile, medical bankruptcies are practically nonexistent in all other developed countries.
Given their utility, these temporary orders to deregulate SOP laws should undoubtedly be made permanent. Returning to past oversight mandates and regulations would blatantly ignore the quality of care provided by NPs and willfully limit their patients’ access to care. At the end of the day, the US population needs better access to healthcare. While removing SOP laws is not a cure-all, it is a cost-effective and low-risk measure to substantially raise the care capacity of the current primary care system.